Weekly Checkup
November 16, 2018
Tackling the IMD Exclusion
Earlier this week, Health and Human Services (HHS) Secretary Alex Azar announced that the Trump Administration will offer state Medicaid programs new opportunities to expand access to mental health treatment through waivers to the IMD exclusion.
The IMD exclusion dates back to 1965 and the birth of the Medicaid program, and like most policies sitting around for over fifty years largely unchanged, it hasn’t aged terribly well. The exclusion prohibits reimbursement for mental health treatment provided by Institutions of Mental Diseases (IMD)—inpatient facilities—with more than 16 beds for Medicaid beneficiaries aged 21 to 65. When it was first instituted, the country was actively working against the inappropriate institutionalization of mental health patients, and restricting Medicaid payments made some sense. Additionally, Congress wasn’t eager to take on the cost of mental health services and wanted to keep them within the purview of states.
The result, however, was an erosion of inpatient mental health treatment capacity, as states failed to provide sufficient funding outside of the Medicaid program and the prohibition incentivized facilities to reduce their total beds in order to qualify for Medicaid reimbursement. Obstacles to repealing the IMD exclusion are primarily two-fold: First, there is still lingering concern about the legacy of institutionalization, but second, the cost associated with Medicaid fully covering inpatient treatment is a significant political and policy problem.
Back in 2015, AAF policy experts proposed possible changes to the exclusion. Those improvements included allowing Medicaid payments for IMD treatment that extend to 30, 60, or 90 days; increasing the IMD psychiatric bed limit to 30 rather than 16; and allowing reimbursement for substance abuse treatment or encouraging state departments of health to apply to HHS for a 1115 innovation waiver that allows Medicaid payments to IMDs.
Since 2015 there have been several administrative actions similar to those policy proposals. The Obama Administration implemented rulemaking in 2016 that allowed Medicaid reimbursement for up to 15 days of treatment in an IMD facility for beneficiaries of managed-care Medicaid programs, though not traditional Medicaid. More recently, the Trump Administration has approved 17 state waivers to the IMD exclusion allowing reimbursement for up to 30 days of substance abuse treatment at IMD facilities, for beneficiaries in either managed Medicaid programs or traditional Medicaid. Similarly, the recently passed SUPPORT for Patients and Communities Act (H.R. 6) temporarily allows states to cover services at an IMD facility for up to 30 days within a one-year period for individuals who have suffered from a substance use disorder for at least a year, without the need for a waiver.
Now, HHS is inviting states to apply for even broader waivers allowing up to 30 days of mental health treatment at IMD facilities through a Medicaid demonstration. While these waivers will need to be budget neutral, they represent a serious effort by the Trump Administration to expand access through the Medicaid program to mental health care and substance abuse treatment. They should be commended.
Chart Review
Tara O’Neill Hayes, Deputy Director of Health Care Policy
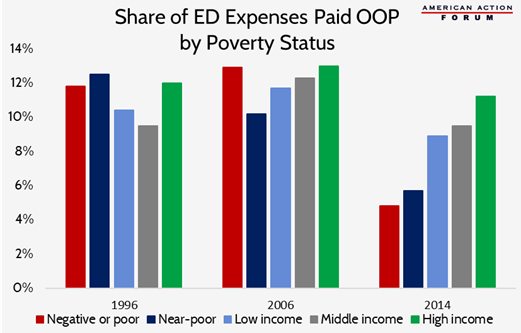
For decades, private insurers in the United States have covered roughly half of all expenses incurred in emergency departments (ED), as shown in this study. Out of pocket (OOP) costs paid by individuals have averaged around 10 percent, but there have been significant differences between income groups, as shown in the chart below. In 2006, the poorest quintile of individuals had the highest OOP costs for emergency room expenses, but those in the next lowest quintile had the lowest OOP expenses. In 2014, following passage of the Affordable Care Act, OOP costs for ED services dropped for all income groups, but most significantly for the lowest income individuals. Now, OOP costs increase as income increases.
Worth a Look
Modern Healthcare: Medicaid OKs Michigan waiver to negotiate drug prices based on outcomes
Politico: California’s new governor embodies Democrats’ dilemma on single payer
Axios: ACA premiums are higher in rural areas