Weekly Checkup
June 7, 2024
Americans Losing the Faith
With new hearings offering retrospectives on the federal handling of the COVID-19 pandemic, an increasing number of Americans are losing trust in the country’s national health authorities and lawmakers and point to a lack of health issue transparency and partisan public health policy as key concerns. Let’s explore this growing trend and talk about what it means for an important aspect of public health policy: trust.
We can start by examining the data. It’s often challenging to gather public sentiment data on a complex issue such as trust, but a recent special report from the Edelman Trust Institute provides some insights. Its report reveals a noticeable drop in the general public’s confidence in national health authorities to “tell the truth about health issues” and “to protect the health of the public.” This drop of over 9 percentage points between April 2022 and April 2023 means that almost half of the American public (48 percent) distrust their national health authorities’ judgment. The study also found that 77 percent of Americans do not trust the government to “do what is right in addressing health needs and concerns,” a drop of 10 percentage points between 2022 and 2023. Additionally, 60 percent of Americans rate the politicization of medical science as their greatest health concern, surpassing care affordability or the threat of another pandemic. These data points underscore the alarming trend of national distrust in health care officials, driven, in part, by the spread of false health information and what many claim is the politicization of medical science.
One could cite any number of well known failures of the public health agencies during the COVID-19 pandemic, but perhaps the most demonstrative such failure was the inability or unwillingness of the Centers for Disease Control and the Department of Health and Human Services’ (HHS) more broadly to change guidance surrounding young child masking. Even when it became clear that such masking was ineffective, and even when it had adverse side effects for young children, federal authorities doubled down on their original guidance, perhaps concerned that it would lose public trust if it was seen to have changed its stance. But refusing to budge is precisely what caused it to lose public trust.
As an aside, as the nation’s trust in government and national health authorities continues to decline, another group seems to be recouping that trust. The Edelman study found that national trust in primary care providers is reaching record highs. A staggering 82 percent of Americans agree with statements such as “I trust primary care providers to tell the truth about health issues and how best to protect the health of the public.”
To rebuild the nation’s dwindling trust in national health authorities, federal health policy must reorient toward the data and away from the pandemic-era political considerations that were responsible for having lost so much public trust. Rather than making partisan-based health decisions, as was both typical and glaring during the past few years, lawmakers and national health authorities should prioritize data-driven findings that provide as much transparency as possible. This won’t always be an easy exercise: Due to the unique and ever-changing nature of what we consider good public health policy, officials must be willing to quickly and efficiently alter health regulations as new findings are verified, rather than waiting for the prevailing political winds to blow before taking necessary action.
It may take a very long time for public health officials to regain the trust of the American people – but it can be rebuilt. It will require our public health agencies to become nimbler, more reactive to the latest scientific data, and of course less reactive to the political fads of the day. While it is a shame that Americans no longer trust our health authorities, the greater shame is that those authorities often made themselves untrustworthy. As Stephen Covey put it, if you want to be trusted, be trustworthy.
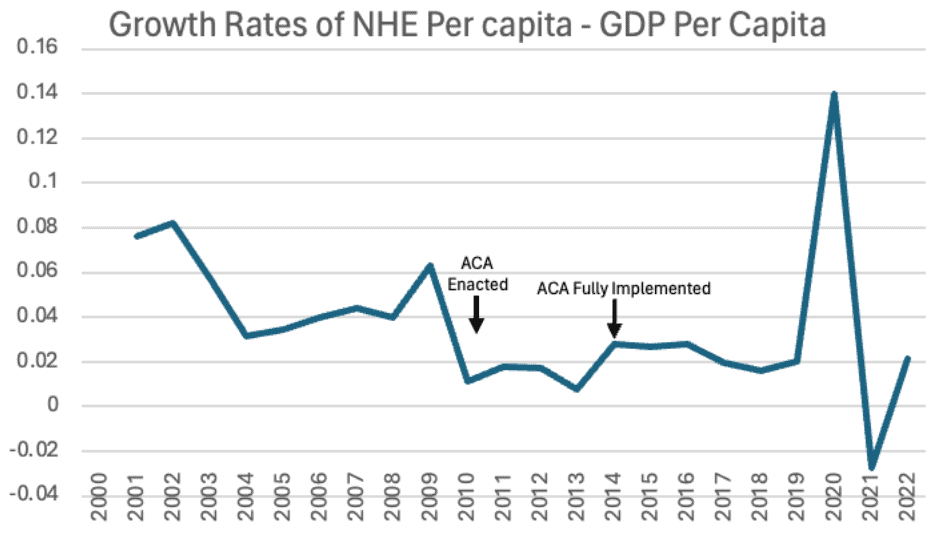
Chart Review: Bending the Cost Curve? A Look at the Impacts of the ACA 14 Years Later
Henry Roberts, Health Policy Intern
A key goal of the Affordable Care Act (ACA) was to bend the health care cost curve. Specifically, the ACA was intended to reduce the growth rate of national health expenditures (NHE) to no higher than the growth rate of the economy (i.e., anything above 0 is “excess cost growth”). But as the chart below shows, 14 years after the ACA’s passage, NHE expenditures continued to rise at rates higher than the per capita GDP growth rate. Between 2010 and 2019, NHE per capita growth rates exceeded GDP growth rates by between 0.75 and 2.79 percent. There is a marked spike in 2020 where GDP fell dramatically as health care expenditures soared due to the pandemic. GDP per capita growth briefly exceeded NHE per capita growth in the period following lockdowns as health care expenditures fell to their pre-pandemic levels and the economy began to rebound. This was due to an anomalous level of GDP growth ushered in by pandemic recovery. Overall, the NHE growth rate does not appear to be converging with the GDP per capita growth rate. Such convergence would be indicated by the curve approaching 0 on the graph below. This lack of convergence indicates that the ACA has effected little to no bending of the cost curve to date.
Sources: