Weekly Checkup
March 15, 2017
The American Health Care Act’s Impact on Medicaid
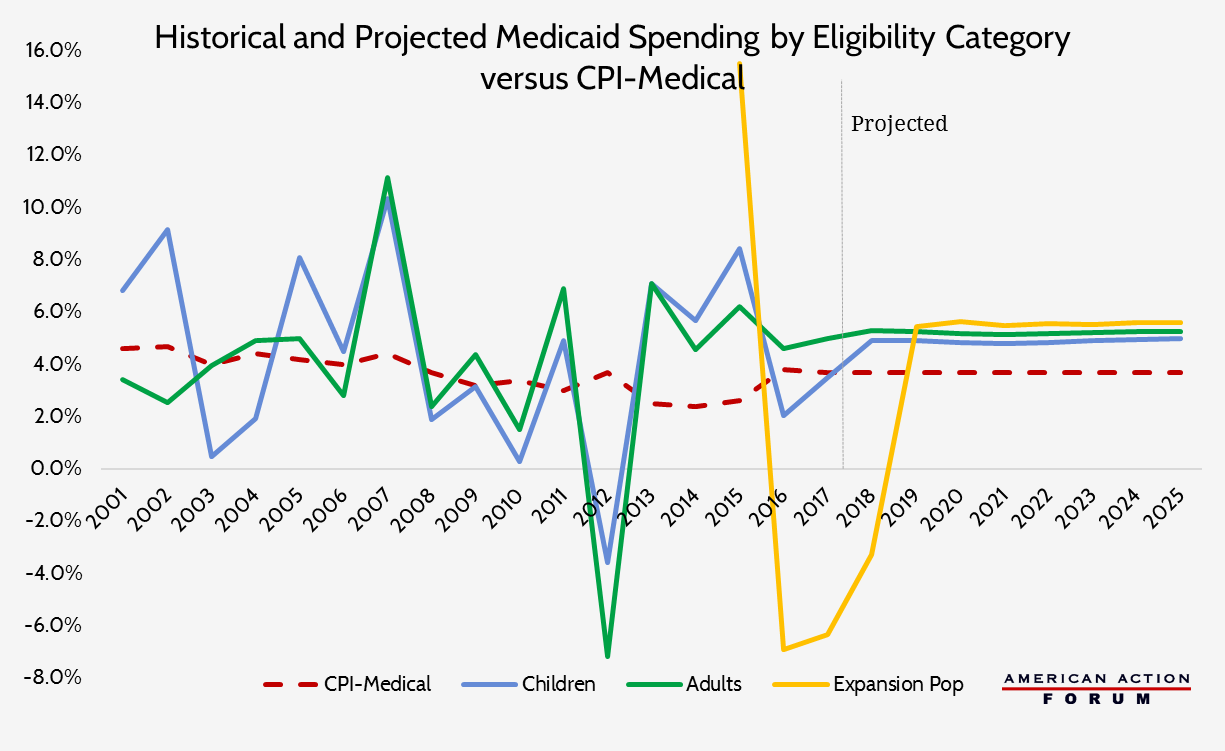
One of the most significant changes to the status quo made by the Republican’s Affordable Care Act replacement, the American Health Care Act (AHCA), is the reform of the Medicaid program. The plan would transition Medicaid from an open-ended entitlement program to one financed through a per capita allotment for each enrolled individual—save for certain vulnerable populations who would be excluded from this change, such as elderly and disabled beneficiaries who qualify for financial assistance. The need for entitlement reform has become more pronounced each year as both health care costs and the populations dependent on these programs continue to rise. Between 2015 and 2025, spending on Medicare and Medicaid is expected to nearly double to $2.2 trillion. The current trajectory for these programs is unsustainable for both federal and state budgets, and beginning next year, Medicare and Medicaid spending is expected to grow faster than spending on private health insurance. The only way to ensure these programs continue to offer benefits to the people who depend on them is to pursue reform. The AHCA’s Medicaid reform would not cap total program spending or the number of people eligible for the program. Rather, beginning in 2020, it would provide states a set amount of funding for each eligible individual enrolled and the funding level would grow at the rate of the medical care component of the consumer price index (CPI-U Medical). The chart below shows historical annual spending growth rates for children, adults, and expansion population adults, as well as the annual growth rate of CPI-U Medical. It is easy to see that such a funding change would simultaneously produce savings without imposing draconian cuts to the program. In fact, some years states would have even been able to save money to put towards future years when spending was higher.