Research
August 11, 2024
Medicare for All: The Harris Plan
In 2019, presidential candidate Kamala Harris designed a replacement for the Affordable Care Act (ACA) using the template of Medicare for All.[1] The replacement (“the Plan” or M4A) is a proposal for a single-payer health program managed by the federal government that has the goal of universal coverage. This report details the findings of the Center for Health and Economy’s (H&E) combined Under-65 and Over-65 microsimulation models on M4A’s impact on health insurance coverage, provider access, medical productivity, and the federal budget. While our estimates are associated with some degree of uncertainty, the summary of our findings is as follows:
KEY FINDINGS:
- Without the need to sign up for insurance and with the promise of all cost sharing and premiums being eliminated, H&E expects universal coverage.
- The health insurance coverage provisions under current law for the non-elderly are estimated to increase federal spending by $43.9 trillion between 2026 and 2035.
- One significant difference in the Harris plan from previous M4A proposals is the explicit funding of health insurance for all undocumented and illegal aliens residing in the United States.[2] The approximate cost of covering an additional 11 million individuals with M4A coverage is $1.8 trillion between 2026 and 2035.
- Under the Plan, medical productivity is projected to decrease by 22 percent for the year 2035 relative to the current baseline due to the massive increase of patients into the health system and the dissolution of network structure.
- Provider access is projected to increase by 19 percent as a result of universal coverage, along with the elimination of cost sharing.
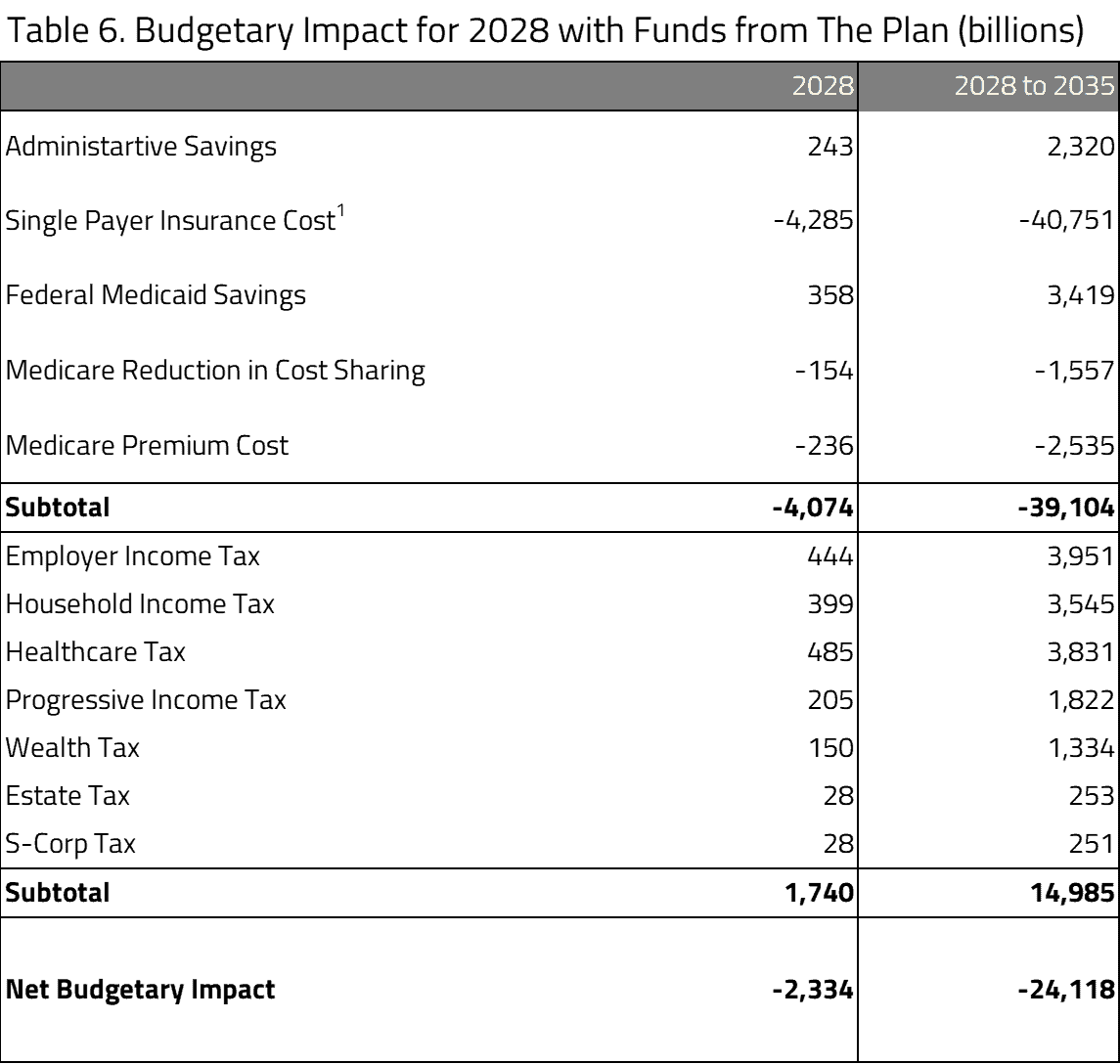
- An additional analysis compares the projected cost with the revenue the Plan expects to see raised. The tax revenue is expected to be about $1.7 trillion; however, this is more than offset by $4.1 trillion in spending, leaving a net federal cost of $2.3 trillion for the year 2028. Over eight years of full operation between 2028 and 2035, the total net cost is $24.1 trillion.
Microsimulation Analysis
This analysis utilizes a microsimulation model developed for use by H&E. The model employs micro-data available through the Medical Expenditure Panel Survey to analyze the effects of health policies on the health insurance plan choices of the under-65 population and interpret the resulting impact on national coverage, average insurance premiums, the federal budget, and the accessibility and efficiency of the health care sector.[3]
The Harris M4A plan, which is scored in this report as taking effect in 2026, is a proposal to introduce a national single-payer health care system. The Plan is meant to fully cover the entire population. All health care costs would be covered by the federal government. Premiums, deductibles, copays, and any other out-of-pocket costs would be completely paid for through federal funds. The Plan proposes to eliminate all other federal health programs, including the private marketplace, and to expand the Medicare program to include the entire population.
Since H&E’s Under-65 Microsimulation Model is a plan-choice model that does not account for the over-65 population, certain assumptions and adjustments had to be made in order to simulate the effects the M4A policy would have. The assumptions made are as follows:
- Similar Actuarial Value: Current Medicare beneficiaries receive insurance with an actuarial value in the 70 to 80 percent range. Therefore, plan choices in the individual and employer market were limited to PPOs that are comparable to the current individual market’s health insurance plans with Gold and Silver (with the costs of cost-sharing loaded) metal levels.
- Total Government Spending: Since the Plan argues for a single-payer system in which all costs to the consumer are eliminated (not including new taxes levied), H&E adjusts by converting all health insurance-related costs into federal spending, or in some cases, lack of revenue.
- Revenue: Since the Under-65 Microsimulation Model only takes into account factors directly related to the health insurance market and many of the pay-fors in the Plan are not related. H&E uses the revenue estimates found in the text of the Sanders plan,[4] which candidate Harris claimed had “good options” to pay for her proposal.[5]
There are several factors not considered in the Harris plan that are outside the scope the microsimulation. First, we do not consider the additional cost of adding a dental benefit to the program since that is not a typical health benefit offered as part of medical insurance. Second, we do not consider the additional cost of adding a vision or hearing benefit to the program. The absence of these benefits will lead to underestimate of the full cost of the Harris plan.
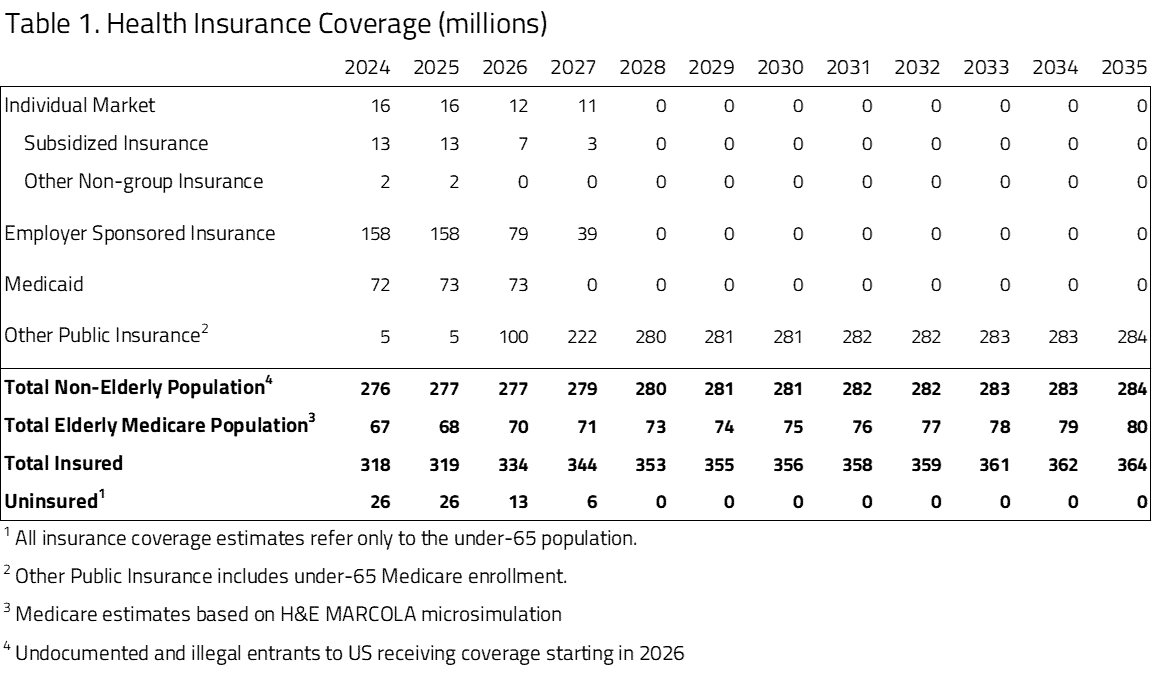
The Harris plan specifies a 10-year implementation period. In an effort to get a cost estimate of the plan when fully implemented, we assume a three-year transition period from 2025 to 2027, with full population transition by 2028 and full cost for program deployment starting in 2026 as seen in Table 1.
Coverage Impact
True to any single-payer health plan, H&E projects there will be full coverage of the population. Since there is no need to sign up for a plan or a program, and anyone can access health care under this plan, complete coverage would be expected. We assume that the entire private insurance market would operate as a public option as proposed by Vice President Harris in 2019 and is accounted for as an expansion of Other Public Insurance. We further assume an additional account of 11 million undocumented immigrants that would be eligible for insurance as proposed by presidential candidate Harris in 2019[6]. As seen in Table 2, we further assume Medicaid will migrate to the federal Medicare option starting in 2027.
Productivity and Access
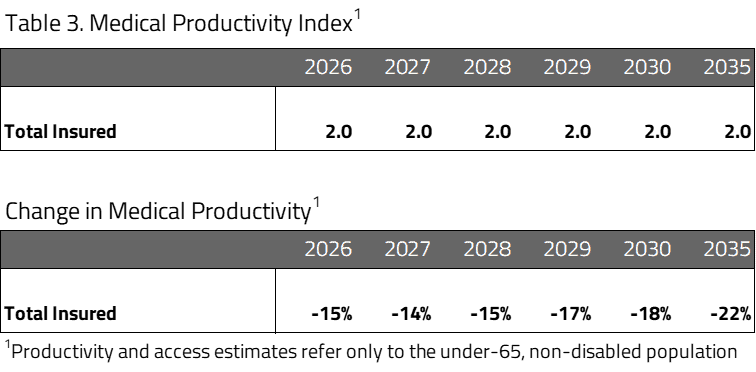
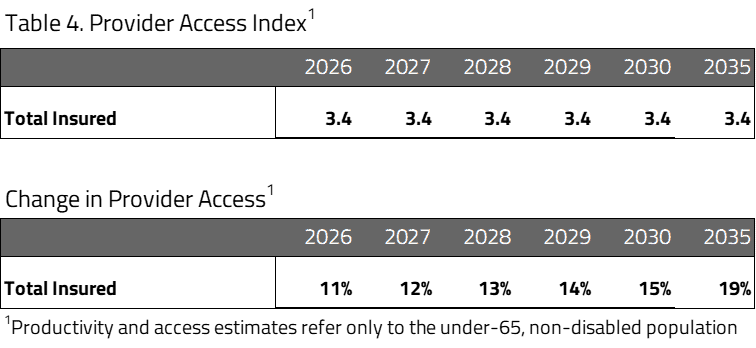
In an attempt to evaluate access and productivity in the health care system, H&E estimates the Medical Productivity Index and the Provider Access Index. Health insurance plan designs are associated with varying degrees of access to desired physicians and facilities, as well as incentives that promote efficient use of resources. H&E estimates each index by attributing productivity and access scores to the range of plan designs available and exploiting changing plan choices to project the evolution of health care quality.
Table 3 describes the net productivity of all insured populations resulting from the Harris plan. H&E expects medical productivity to decrease under M4A. The influx of the previously uninsured into the market, along with the dissolution of the network structure, leads to a decrease in efficiency. Also, a market-based system typically leads to more efficiency, as individual market plans require cost-sharing, which encourages price-conscious decision making among patients. The elimination of a health insurance marketplace – and therefore any price-conscious decisions due to cost-sharing – also contributes to the decrease in productivity.
Table 4 describes the net provider access of all insured populations resulting from the Harris plan. Under the Plan, average provider access is projected to increase relative to current law due to the global coverage instituted by single-payer insurance. H&E also projects an increase in average provider access for the total insured population as a result of lower enrollment in Medicaid, which generally offers poor access to physicians. This projection assumes there is adequate provider supply.
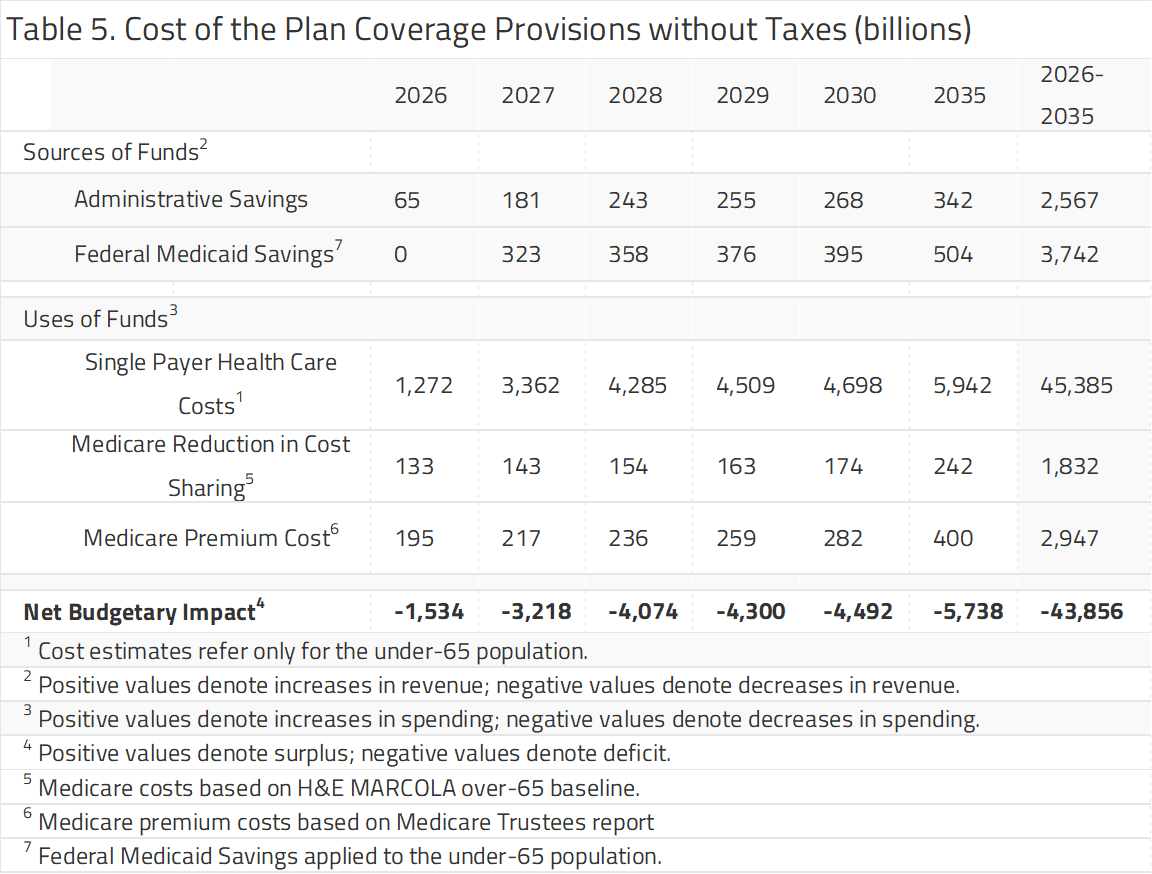
H&E projects that the insurance coverage expansion under the Plan has a net budgetary impact of -$43.9 trillion dollars over the next decade. The budget impact table is divided into two sections: “Sources of Funds” refers to changes in dollars raised by the federal government and “Uses of Funds” refers to changes in dollars spent by the federal government.
Over the decade spanning between 2026 and 2035, H&E estimates that non-elderly coverage provisions under the proposal will cost $45.4 trillion. The yearly cost is expected to begin at around $4.3 trillion in 2028 (with full implementation) and increase to $5.9 trillion in 2035. This is prior to accounting for administrative savings to the federal government of $2.6 trillion over 10 years. These savings would come from the elimination of federal personnel and contractors required to operate health benefits for Medicaid, SCHIP, TriCare and other federally financed health insurance programs. We include additional savings that we expect to result from the reduction of costs associated with individual and employer sponsored health insurance markets. We account for the proposed additional costs of reducing beneficiary cost sharing in the existing Medicare program as was specified in the Sanders M4A plan and implied in the Harris plan.
We estimate those additional costs to remove Medicare cost sharing to be $133 billion in 2026 and $1.8 trillion from 2026 to 2035. Similarly, we also add in the cost of Medicare premiums that will no longer be collected under the Plan, given Sanders would have replaced the current premium structure with a 4 percent tax on incomes over $29,000 (included in offsets under table 6), of which Harris specified her only difference was in exempting households with incomes up to $100,000.
In its analysis of a proposal’s impact on the federal budget, H&E looks only at provisions directly related to health insurance coverage.
As noted above, one significant difference in the Harris plan from previous M4A proposals is the explicit funding of health insurance for all undocumented and illegal aliens currently in the United States. Our current model has assumed there are 11 million illegal aliens in the United States and has counted them as uninsured. This is the most recent number reported by the Office of Homeland Security Statistics and reflects estimated unauthorized immigrants as of January 2022.[7] This is likely an underestimate given the recent influx of encountered and entered reported by the U.S. Customs & Border Protection totals over 10 million from 2021 to 2024.[8] The approximate cost of covering an additional 11 million people with M4A would be $1.8 trillion between 2026 and 2035 assuming no further additional illegal alien encounters from 2026 on.
UNCERTAINTY IN THE PROJECTIONS
The Center for Health and Economy uses a peer-reviewed micro-simulation model of the health insurance market to analyze various aspects of the health care system.[9] As with all economic forecasting, H&E estimates are associated with substantial uncertainty. While the estimates provide a good indication on the nation’s health care outlook, there is a wide range of possible scenarios that can result from policy changes, and current assumptions are unlikely to remain accurate over the course of the next 10 years. Importantly, this uncertainty does not lead to biased results. H&E attempts to depict an unbiased, middle-ground representation of the future should the policy and economic environment remain constant. While the goal is to project the most likely scenario, actual events may differ significantly from published predictions.
With a proposal that puts forward substantial changes, there are bound to be myriad uncertainties when projecting different scenarios. There are three of these that will be brought up in the discussion: the magnitude of health care usage in such a system and the complications that may bring and certain cost effects that may arise from the Plan; certain proposals that the model is unable to score; and the effects of the pay-fors that are included in the Plan.
M4A proposes a drastically different system that leads to many different assumptions for a plan choice model such as H&E’s Under-65 Microsimulation Model. Among those assumptions is the usage of insurance. Since the Plan proposes to eliminate premiums and all cost sharing, it is highly likely that health care usage will go up – which is confirmed by the decrease in provider access above. Yet the magnitude of that increase is up for debate and increases the uncertainty involved in these estimates.
Next, the Plan has a few policies that H&E is simply unable to account for: Funds raised by progressive income tax rates, taxing capital gains and dividends, and estate tax, among others, currently fall outside the realm of H&E’s ability. While H&E has the ability to score things such as the individual income-based premium, to avoid confusion, it was left out of the budget impact assessment. In order to provide a glance at what the budgetary impacts of these taxes might be, see Table 6. H&E used the numbers provided in the text of M4A and applied them to the budget for the year 2028.
As seen in the table, after the revenues the writers of the Plan calculated are added to the baseline for 2028, the net budget shortfall remains about $2.3 trillion dollars. Though this is a rough picture of what 2028 might look like with the Plan’s projected revenues, the number indicated for the net budgetary impact is a substantial amount to overcome. Over eight years of full operation between 2028 and 2035, the total net cost is $24.1 trillion. Outside of the health care budget, the impact of seeking to break even through increased taxes would be challenging on the economy at large.
[1] https://kamalaharris.medium.com/my-plan-for-medicare-for-all-7730370dd421
[2] While there has been debate over whether candidate Harris meant she would cover undocumented immigrants for free, her health care plan provides health care to enrollees for free and she explicitly stated she would include and would not discriminate against undocumented immigrants. Therefore, we treat undocumented immigrants just like any other enrollees in the Harris Plan.
[3] https://healthandeconomy.org/2017-project-a-winning-alternative-to-obamacare/#_ftn2
[4] https://www.sanders.senate.gov/wp-content/uploads/options-to-finance-medicare-for-all.pdf
[5] While candidate Harris proposed limiting the impact of the Sander’s 4% tax on income for households making under $100,000, she proposed replacing the revenue with a tax on stock trades and derivative transactions. Given the intent was to provide revenue roughly in line with Senator Sander’s offsets, we maintain his overall revenue estimates.
[6] https://www.youtube.com/watch?v=O-QP5TBTVhY
[7] https://www.dhs.gov/sites/default/files/2024-05/2024_0418_ohss_estimates-of-the-unauthorized-immigrant-population-residing-in-the-united-states-january-2018%E2%80%93january-2022.pdf
[8] https://www.cbp.gov/newsroom/stats/nationwide-encounters
[9] Parente, S.T., Feldman, R. “Micro-simulation of Private Health Insurance and Medicaid Take-up Following the U.S. Supreme Court Decision Upholding the Affordable Care Act.” Health Services Research. 2013 Apr; 48(2 Pt 2):826-49.